Who your money helps
100% of the money that you raise for Stand Up To Cancer will help people and their families by tackling cancer from all angles.
People like Rochelle and her sisters, who lost both their parents to cancer. People like Lottie, who is training in cancer research to smash cancer with science. People young and old, across the country joining forces to overthrow cancer and get treatments to those people who need them, faster.

The gloves are on. Lottie's showing cancer who's boss.
Lottie’s dad sadly lost his fight against cancer, but now Lottie is working to kick cancer where it hurts.
Lottie, 23, joined the rebellion against cancer when she saw her dad receive treatment as part of a clinical trial. Studying neuroscience at the time, she made the decision to move into cancer research. The money you raise will help fund clinical trials and super-scientists working on new treatments and cures.
“I think about Dad a lot when I am doing extra work or staying up to finish projects. I think about him and other people’s dads – hopefully we can help them.”
Oliver's shown cancer what he's made of. And won.
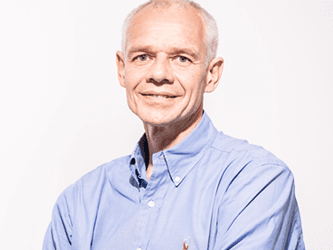
Father-of-one Oliver, 53, was diagnosed with mouth cancer in 2009 after spotting a lump in his neck under his jaw. Oliver took part in a Cancer Research UK clinical trial that used targeted radiotherapy to treat his cancer. He’s taken on cancer and shown it what he’s made of.
“I Stand Up To Cancer for me and the other people I saw during treatment. Those people on the wards – they inspire me. Young, old, everyone. We all need to rebel against cancer.”
Cancer took Rochelle's parents. Cancer's time is up.

Rochelle, 27, and her sisters have lost both their parents to cancer. Her dad died of pancreatic cancer when she was just 14 and her mum was diagnosed with a terminal brain tumour when she was 25. She moved back home to look after her mum and her two younger sisters until her mum’s death in 2012.
“I think that cancer is something that can be stopped – we have the potential to stop it. If everyone comes together and lends their support, you can stop people going through what we went through.”
Laurel stands up to cancer. Every day.

After experiencing difficulty swallowing, mum-of-three Laurel, 60, was diagnosed with oesophageal cancer.
“It was a shock and the treatment was tough but I’m a different woman since I had cancer. I’m a million times more positive. I see the best in everything and I love life. I Stand Up To Cancer on a daily basis.”
Laurel’s daughter Kelly says “I am so grateful mum is still here – she is an inspiration. Every mother’s day, birthday or Christmas is so special.
"It had been such a difficult time for all of us and we had all been there together. Everyone should support Stand Up To Cancer as it’s helping families like ours.”
How you can help
Fundraise for SU2C
Sign up to get your free fundraising pack, full of epic ideas and handy tips to get you inspired to raise some serious cancer-crushing cash.
Make a donation online
Or call 0300 123 9024 to make a payment by credit or debit card. (Standard geographic charges from BT landlines will apply. Calls from other network operators and mobiles may cost more.)